Antibiotics can be life-saving, but some carry a much higher risk of triggering Clostridioides difficile (C. diff). On this page, you’ll learn which antibiotics are most linked to C. diff, which are generally lower-risk, who’s most at risk after antibiotics, and the key questions to ask before you fill your next prescription.
What Is C. diff & Why Antibiotics Trigger It
C. diff is a bacterium that can live harmlessly in some people, but antibiotics can disrupt your normal gut flora (the “good” bacteria) that normally keep it in check. When that balance is lost, C. diff can multiply and release toxins that lead to diarrhea, cramping, and—in some cases—serious colitis.
Think of your gut like a garden: the helpful plants (your good bacteria) keep weeds down. A broad antibiotic can act like a strong weed-killer—it takes out the weeds and many of the flowers—leaving bare soil where the C. diff “weeds” can take over.
Not all antibiotics act the same or cover the same range. Broad-spectrum antibiotics wipe out many kinds of bacteria at once; narrow-spectrum antibiotics target a smaller set. That breadth is one reason some drugs carry higher C. diff risk than others.
Top 5 Antibiotics Most Linked to C. diff
These categories show up repeatedly in large studies and real-world reports.
| Antibiotic / Class | Common Examples | Typical Uses | C. diff Risk Signal |
|---|---|---|---|
| Clindamycin | Clindamycin, Cleocin | Dental, skin/soft-tissue, ENT | Highest association (>8× vs doxycycline) |
| Fluoroquinolones | Ciprofloxacin (Cipro), levofloxacin, moxifloxacin | UTI, respiratory infections | High (numerous studies & patient reports) |
| 3rd/4th-Gen Cephalosporins | Cefdinir, cefuroxime, ceftriaxone, cefepime | Respiratory, ENT, inpatient empiric therapy | High (broad spectrum → more gut disruption) |
| β-lactam/β-lactamase inhibitor combos | Amoxicillin-clavulanate (Augmentin), piperacillin-tazobactam (Zosyn) | Outpatient ENT/respiratory; inpatient broad coverage | High (esp. Augmentin in outpatient use) |
| Carbapenems | Meropenem, ertapenem, imipenem-cilastatin | Serious inpatient infections | High (very broad spectrum) |
Key evidence: Zhang et al., 2022 (U.S. outpatient claims, ~36 million records); Brown et al., 2021 (course length & risk).
Lower-Risk Antibiotics (Not Zero-Risk)
Some antibiotics are generally associated with lower C. diff risk in studies. Lower risk doesn’t mean no risk—especially with repeated or prolonged use.
| Antibiotic / Class | Common Examples | Typical Uses | Notes on C. diff Risk |
|---|---|---|---|
| Tetracyclines | Doxycycline, minocycline | Skin/soft-tissue, acne, tick-borne | Among the lowest association in analyses |
| Nitrofurantoin | Macrobid, Macrodantin | Uncomplicated UTI | Lower association vs broad agents |
| Trimethoprim-sulfamethoxazole | TMP-SMX (Bactrim, Septra) | MRSA skin infections, UTI | Lower than high-risk classes; not zero |
| Linezolid | Linezolid (Zyvox) | MRSA, resistant gram-positive infections | Not a top trigger in outpatient data |
| Vancomycin (IV) | Vancomycin | Serious MRSA infections (IV); oral vanco treats C. diff | Not a top cause of C. diff |
Key evidence: Xu et al., 2022 (doxycycline lower association); Zhang et al., 2022 (comparative outpatient risk).
Course Length, Repeats & Relapse Risk
Risk isn’t just about which drug you take — it’s also about how long you take it and whether you’ve had multiple courses recently.
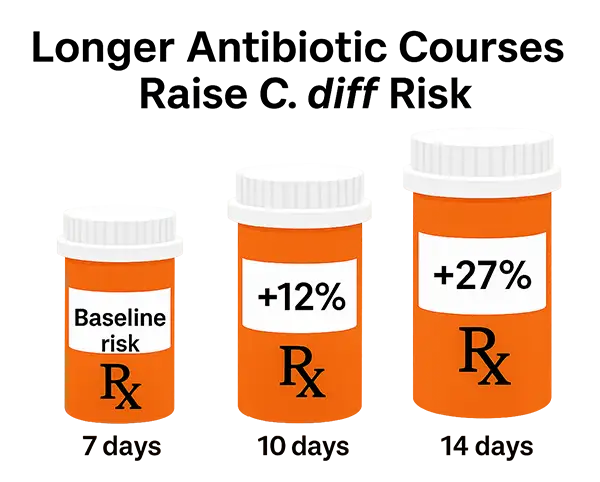
A Canadian case-cohort study found 10-day courses increased C. diff risk by ~12% and 14-day courses by ~27% vs 7-day courses, with risk compounding across repeated exposures.
The danger climbs even higher with repeated courses of antibiotics. Each new prescription disrupts your gut a little more, and the odds of relapse stack higher every time.
Key evidence: Brown et al., 2021 (Clinical Infectious Diseases).
Who’s Most at Risk After Antibiotics
- Prior C. diff infection: strongest predictor of recurrence; risk remains elevated for weeks after treatment.
- Older age (65+) and/or significant medical conditions.
- Recent hospitalization or nursing home exposure.
- Stomach acid suppression (PPIs) and certain other medications.
- Recent or repeated antibiotics (especially high-risk classes above).
Importantly, the danger doesn’t end the day you stop an antibiotic—the risk window remains elevated for up to 3 months afterward, especially with higher-risk drugs.
Key evidence: Hensgens et al., 2012 (risk highest during therapy and up to 3 months after).
Key Takeaways & Questions to Ask Your Provider
- Not all antibiotics carry the same C. diff risk—some are much higher than others.
- Shorter, targeted (narrower-spectrum) courses generally mean less gut disruption.
- Your personal risk depends on age, history (especially prior C. diff), setting, and medications.
Questions to ask your healthcare provider (doctor, surgeon, dentist, or oral surgeon)
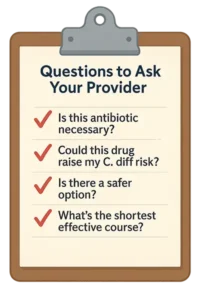
- “Is this antibiotic really necessary right now?”
- “Could this drug increase my risk for C. diff infection?”
- “Is there a safer option or a narrower-spectrum option that would still work?”
- “What’s the shortest effective course for my situation?”
- “Should we do a culture or susceptibility test first?”
- “What side effects and precautions should I know about for my gut?”
- “Can I review the plan at home before deciding?”
Alignment: IDSA/SHEA clinical guidance emphasizes risk factors and treatment choices; a good clinician will be familiar with current recommendations.
Final Thoughts
And just to be clear — the antibiotics linked with higher C. diff risk aren’t necessarily “bad” drugs — sometimes they’re exactly the right choice. What matters is knowing the risks, asking good questions, and working with your provider to choose wisely.
One more thing to remember: Don’t overlook dental antibiotics. Dentists account for a surprising share of antibiotic prescriptions, and up to 15% of C. diff cases have been linked to them. If your dentist or oral surgeon suggests antibiotics, ask if it’s truly necessary, or if a lower-risk option could work instead.
What to Read Next
If antibiotics are the number one cause of C. diff, then probiotics are one of the most powerful ways to start restoring balance afterwards. Not all probiotics are the same though — some strains simply don’t survive the gut, while others have been studied specifically for C. diff recovery.
Discover the best probiotics for C. diff recovery and which ones stand out for rebuilding gut health after antibiotics.

About the Author – Michelle Moore, BSc
Michelle Moore is a microbiologist, holistic health educator, and author of C. difficile Treatments & Remedies. With over 10 years of experience in pharmaceutical research and over 20 years in natural medicine, she helps people overcome C. difficile and other chronic infections naturally.
