Probiotics are living microorganisms that should benefit your health when you take them. Probiotics can help restore good microbes in the gut and they work in a number of different ways to help keep you, your immune system and your gut flora healthy. However, many people have found probiotics don’t help them with C. difficile. There are good reasons why probiotics often don’t work, as you’ll discover below.
The Root Cause of C. difficile
C. difficile infections result from an overgrowth of C. diff. bacteria inside your intestines. The most common trigger for a C. diff. infection is antibiotic drugs. When you take antibiotics, they indiscriminately kill the protective bacteria in your gut. Once these friendly gut bacteria are killed, they can no longer compete against the C. diff. bacteria, which results in a C. diff. overgrowth and infection.
The answer for C. diff. lies in reversing how the problem was created in the first place. A big piece of the puzzle is to restore a healthy microbial balance in the gut. However, all probiotics are not created equal, especially for C. difficile infection support.
New Research Reveals Surprises
 Recent discoveries by the Human Microbiome Project (HMP) have given us great insight about what microorganisms live within us and how they work together to create a healthy gut. And new research reveals how your gut microbiome, which is all the species of microorganisms living inside you, has a huge effect on your health, especially with infections.
Recent discoveries by the Human Microbiome Project (HMP) have given us great insight about what microorganisms live within us and how they work together to create a healthy gut. And new research reveals how your gut microbiome, which is all the species of microorganisms living inside you, has a huge effect on your health, especially with infections.
An astounding 70-80% of your immune system’s function is directly related to the health of your GI tract and your microbiome. So far, several thousand different species of bacteria, fungi and other microorganisms that make up your microbiome have been discovered by the HMP1. The different species communicate with each other and share information to survive. Your microbiome also helps you to digest food, absorb nutrients and produce vitamins and enzymes. And importantly, your microbiome is your first line of defense against infections.
The HMP also made some surprise discoveries. They found that C. diff. is a normal inhabitant of the GI system in many people and it causes no problems. In healthy people, the other microorganisms inside your gastrointestinal system compete with C. diff. bacteria for food and space, keeping the C. diff. in balance.
A healthy gut is a diverse gut that has many different kinds of microbes, including low levels of C. diff. bacteria.
Also of interest, the HMP found that the popular Lactobacillus species only make up 1% of the total microbes in the human gut2. While Lactobacillus is only a small portion of the human gut microbiome, it’s the number one species used to make probiotic supplements. This discrepancy may help explain why probiotics provide little help for many people. See more about probiotic issues here.
Disruption of Gut Bacteria Tied to Chronic Diseases
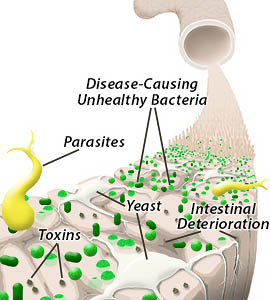
Unhealthy intestines can harbor toxins, parasites, harmful yeast species and overgrowth of disease-causing bacteria, including C. difficile.
The HMP studied the differences between healthy and diseased gut flora. They found that your microbiome can be harmed by medications such as Advil, Motrin and especially antibiotics. Poor diet, chlorinated water, stress and toxins in food, such as weed killers like glyphosate, can also harm your microbiome.
Why You Need Probiotics for C. diff.
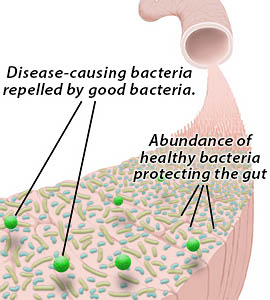
Good bacteria coat and protect the intestinal wall, inhibiting and repelling unhealthy bacteria and maintaining intestinal health.
Restoring balance to your gut is the key to long term success with C. difficile. The majority of scientific studies have shown positive results when adding probiotics along with antibiotics for treating C. difficile3, 4. Taking probiotics before you start taking an antibiotic regimen has also been shown to help prevent C. difficile.
The simplest way to get the probiotics you need is by taking a supplement. But most probiotic supplements are killed by your stomach acid before they reach your intestines. If you already have C. difficile, taking a targeted, true probiotic is one of the best things you can do to speed your recovery.
Choosing the Right Probiotic for Targeted Support

Most probiotics only reseed your gut. They don’t “pull the weeds” or “tend the soil” of your microbiome.
If your gut microbiome was a flower garden, then these species would act like seeds. Reseeding may grow new flowers, but it won’t “pull out the weeds” or reduce disease causing bacteria. Reseeding also fails to “tend the soil”, or heal your gut tissues and neutralize toxins in the gut.
Several Bacillus probiotic species are ideal for gut restoration and immune support as they meet all five requirements for a true probiotic. Bacillus species have anti-inflammatory and immune stimulation properties in the gut and they also promote gut tissue healing and policing of the gut for disease-causing organisms like C. difficile. Because of their many benefits and long history of use, Bacillus species are a great option for long term prevention as well as short-term infection support.

True probiotics benefit your microbiome in multiple ways by reseeding, “pulling weeds” and “tending the soil”.
Using the same analogy of a flower garden, Bacillus and Sac. boulardii work in multiple ways to keep your garden healthy and thriving. Bacillus and Sac. b. actually “recondition” the gut by “fertilizing” and tending the soil, meaning they promote the growth of your resident healthy bacteria. They also “pull out the weeds” by reducing unhealthy bacteria. Bacillus “tends the soil” by healing tissues, removing some bacterial toxins, boosting your immune system and aiding digestion and nutrient absorption. Learn more about this revolutionary probiotic here.
Not all Probiotics are Created Equal
Taking the right kind of probiotic is essential. Probiotics must be both potent and stable to handle your stomach. They should also contain the correct species of bacteria or yeast that will live in and positively effect your microbiome in order to assist your healing. Delivering the right strain of probiotic with enough potency has always been a problem in the probiotic industry.
Taking probiotics is an easy and effective way to support your microbiome and immune system and to speed infection recovery.
Probiotics are especially important if you have a history of recurring C. diff. infections. If you have taken antibiotic drugs recently, then probiotics can help reduce the negative side effects and help repair damage done by these drugs. Even if you don’t have an infection, daily probiotic use can help your body maintain a balance of healthy microbes, which improves your overall health and helps prevent future infections.
- They survive the acidic stomach at 100%
- They actually will thrive and make a home in the human gut (amazingly, many probiotics do not)
- They aren’t killed by antibiotics like most probiotics
- They inhibit the growth of C. diff. bacteria and other pathogens
- They enhance the immune system and produce antioxidants and vitamins in the gut
- They can survive with or without oxygen
- They are widely used in Europe and are safe and effective
Why not use a true probiotic that also combats C. difficile? Using a true probiotic promotes the growth of healthy gut flora and targets pathogens making it another effective arm of your treatment approach.

About the Author – Michelle Moore, BSc
Michelle Moore is a microbiologist, holistic health educator, and author of C. difficile Treatments & Remedies. With over 10 years of experience in pharmaceutical research and over 20 years in natural medicine, she helps people overcome C. difficile and other chronic infections naturally.
References
- A framework for human microbiome research, The Human Microbiome Project Consortium, Nature 486, 215–221 (14 June 2012).
https://www.nature.com/nature/journal/v486/n7402/full/nature11209.html - Heeney, Gareau, Marco. Intestinal Lactobacillus in health and disease, a driver or just along for the ride? Curr Opin Biotechnol. 2018 Feb; 49: 140–147.
- Recommendations for probiotic use – Floch et al, J Clin Gastroenterol. 2008 Jul.
- Probiotics for the prevention of Clostridium difficile-associated diarrhea in adults and children, Joshue Z Goldenberg et al, 31 MAY 2013 The Cochrane Library.
Image credits: Bacteria combo graphic ©CDC and ©Lester Moore, Human tree ©freshidea/Fotolia, Supplement bottles ©Elenathewise/Fotolia, illustrations ©Lester Moore




 Fill in the form below to get our C. diff. tips newsletter and your free report “10 Things You Need to Know to Overcome C. difficile”.
We value your Privacy. Your email will be kept strictly confidential & secured. See our
Fill in the form below to get our C. diff. tips newsletter and your free report “10 Things You Need to Know to Overcome C. difficile”.
We value your Privacy. Your email will be kept strictly confidential & secured. See our