Skip below to the following sections:
Why is C. difficile so Challenging?
Why Antibiotics Fail
The Problem with Fecal Transplants
3 Pitfalls of Alternative Remedies
New Herbal Blends for C. difficile
Michelle’s Recommended Herbal Blends for C. difficile
Get Special Savings
Why is C. difficile so Challenging?
When C. difficile bacteria grow out of control, they release toxins that cause diarrhea, colitis and gut inflammation.
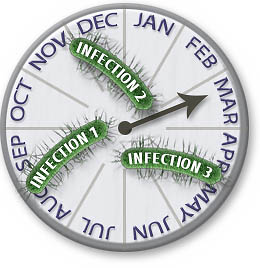
- C. diff. bacteria are very clever at surviving. They are hard to kill, they evade antibiotics and they are adept at causing recurring infections.
- The treatments we rely on for C. difficile often fail. And even when these treatments work, they do nothing to stop the infection from coming back later.
C. difficile bacteria are complex living organisms with powerful survival skills. Bacteria learn and evolve over time and they communicate with each other in order to survive. Bacteria also have multiple ways to evade, counteract and hide from the treatments we use to kill them. Below are the main tactics C. difficile can use to survive and repel antibiotics.
Biofilms
Biofilms are clusters of bacteria that hide within a tough, protective, gluey matrix. These biofilms stick to body tissues like the lining of your gut and they shield the bacteria from being detected by your immune system. Biofilms also shield bacteria from attack by antibiotic drugs2. In fact, most antibiotics are thousands of times less effective against biofilm bacteria as opposed to free-floating bacteria. Taking antibiotics for biofilms is like shooting arrows at a brick wall. Once you stop taking the antibiotics, the bacteria leave the biofilm to cause another infection. If you’ve struggled with recurring C. diff. infections, then there’s a good chance that biofilms are involved.
Efflux pumps
When C. difficile bacteria are attacked by an antibiotic drug, they turn on tiny pumps that kick the antibiotic out. These efflux pumps expel the antibiotic from within the bacteria cells, allowing it to survive. Efflux pumps evolve and become smarter over time and are a major cause of antibiotic resistance. What would otherwise be a lethal dose of antibiotic is expelled from the bacteria, allowing it to survive3.
Quorum SensingBacteria like C. difficile use chemical signals called quorum sensing to communicate with each other and resist antibiotics. If one bacteria senses a danger, it can send warning signals to neighboring microbes. This allows different bacteria to coordinate to protect each other. A similar type of communication is called plasmid exchange and it can even occur between different species of bacteria. And the more the bacteria are exposed to antibiotics, the quicker they learn how to resist them.
Spores
Spores are kind of like an apple seed. Seeds are able to withstand harsh temperatures and conditions and you can store them for long periods of time. A seed remains dormant until it meets soil and water, then it starts to grow into an apple tree.
C. diff. spores work just like seeds. Spores have several layers of protective armor that surround the vital parts of the bacteria inside the core. Spores shield C. diff. from treatments and allow it to survive in a dormant state for long periods of time. When conditions are right, the spores can revert to an active form and cause another infection. C. diff. spores can even survive on surfaces in your home or on your clothing for months.
Biofilms, spores and other survival strategies are a normal part of the C. difficile life cycle. But when you take antibiotics, the drug stresses the bacteria and causes them to make spores or biofilms for protection. The active form of C. diff. may be killed by the antibiotics, but the spores and biofilms let C. diff. hide inside your gut, waiting until the coast is clear to become active again. So biofilms, spores and other resistance methods are a key reason why C. diff. is so difficult to treat with antibiotic drugs.
Why Antibiotics Fail
For nearly a century, mainstream medicine has been at war with bacterial infections. Drug companies race to develop new antibiotics before bacteria learn how to resist them. But it’s a war we are slowly losing. Each year, deadly bacteria become more and more resistant to the only treatments that mainstream medicine has to treat them. Some of these so-called “superbugs” are resistant to every known antibiotic drug. The slowing pace of new antibiotic development, plus mainstream medicine’s ignorance of alternatives, creates the perfect storm for superbugs to thrive and spread.
Despite their problems, antibiotics are still an important treatment for infections. These drugs often work very quickly and effectively to stop an infection. But these powerful drugs have many downsides you should be aware of before using them, as detailed below.
Side EffectsTaking antibiotics is like dropping bombs on a garden to remove the weeds. These are dumb bombs, without any guidance systems. It’s a hit and miss strategy, dropping multiple bombs, trying to get one to hit the target. Even if you score a direct hit, the explosion causes a lot of collateral damage to your garden. And once the bombing raid stops, your garden is left in shambles, with more weeds growing back than you started with.
Your body is like the garden. Doctors routinely prescribe one antibiotic after another, a hit and miss strategy to find a drug that works. Even if an antibiotic works, it causes negative side effects and collateral damage to your body. Antibiotics wipe out the good bacteria in your gut along with the bad ones. So once you stop taking the antibiotics, the C. diff. infection often returns.
Other secondary infections may strike after taking antibiotic drugs, such as yeast or Candida. And antibiotics frequently cause many side effects, including nausea, diarrhea, dehydration, rashes and other allergic reactions and organ dysfunction.
Standard Protocol Treatments
Despite all their downsides and limitations, antibiotic drugs are still the “standard protocol” treatment for bacterial infections. And your doctor is not likely to prescribe any kind of antibiotic alternatives, no matter how safe or effective they may be. Your doctor is under great pressure to stick with standard protocol treatments only. That pressure comes from the healthcare system, insurance companies, drug companies, medical boards and state government agencies who may threaten to revoke a doctor’s license for deviating from the standard protocol.
So in the mainstream healthcare system, antibiotics are the only treatment option you’ll likely get for C. difficile. The trouble, only a few antibiotics have any effect on C. diff. infections. And each year these drugs become less effective because of antibiotic resistance.
Antibiotic ResistanceAntibiotics are simple molecules that are easy for bacteria to figure out and resist. In contrast, bacteria like C. diff. have complex survival and resistance mechanisms that constantly learn, change and improve themselves.
In short, bacteria are smart and antibiotics are dumb.
A good example of antibiotic resistance is Flagyl, a.k.a. metronidazole. Just a few years ago Flagyl was the first line, standard protocol treatment for C. difficile. But because of antibiotic resistance, Flagyl is no longer a reliable treatment. The newer antibiotics vancomycin and fidaxomicin are now the first line treatments for C. diff. But how long will the newer drugs last before resistance renders them useless too?
Antibiotics Promote Recurring InfectionsOne of the biggest problems with antibiotics is they fail to fix the root cause of C. difficile, which is an imbalance in your gut flora. In fact, antibiotics actually contribute to recurring infections because they wipe out your good gut flora and weaken your immune system.C. diff. often recurs weeks or months after you stop taking antibiotics.
Antibiotics also do nothing about the toxins that C. difficile creates inside your gut. These toxins cause the colitis, diarrhea and many of the worst symptoms of C. difficile.
The bottom line is that antibiotics just don’t cut it. They may help for a while, but they can make matters worse in the long run. Many people find themselves in a downward cycle of antibiotics, reinfection, more antibiotics, more reinfections, etc. Yet antibiotics are the only options offered by mainstream medicine, with the single exception of fecal transplants, which have problems of their own.
The Problem with Fecal Transplants
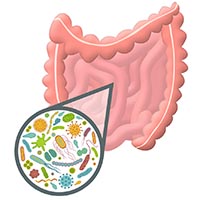 The only alternative to antibiotic drugs for C. diff. offered by mainstream medicine is Fecal Matter Transplantation, or FMT. This treatment attempts to fix your imbalanced gut flora by borrowing healthy gut flora from a donor’s stool.
The only alternative to antibiotic drugs for C. diff. offered by mainstream medicine is Fecal Matter Transplantation, or FMT. This treatment attempts to fix your imbalanced gut flora by borrowing healthy gut flora from a donor’s stool.
FMT offers many advantages over antibiotic drugs. It can be 90% effective in the short term 4. And unlike antibiotics, it’s relatively free from obvious side effects. And there are new FMT methods that use artificial stool, rather than stool from a human donor. But FMT is not without its risks and shortcomings.
Mixed FMT ResultsResults are often temporary with FMT. Some patients get recurring C. diff. after FMT, even without taking antibiotic drugs. If FMT is unsuccessful, patients have to get another FMT or take antibiotics5.
Even after an FMT, your microbiome may eventually revert back to its old state. Unless you change the conditions that caused your microbiome to become imbalanced in the first place, it may revert back to how it was before the FMT. These conditions that determine your microbiome include your diet, stress levels, genetics, your environmental exposures and other factors that make each person’s microbiome unique, just like a fingerprint.
Potential RisksOne study indicated that a FMT recipient’s temporary fever and elevated CRP levels (a marker for inflammation) were tied to toxins that were transferred from the donor’s fecal matter6. Another study indicates that if you receive an FMT and then later take antibiotics, you may have a triple risk of recurring C. diff. infection after antibiotic use7.People have thousands of different organisms in the gut flora, so you never know what you’re getting with traditional fecal transplants.
When you receive stool from a donor, you never really know what you’re getting. Scientists still know very little about the human gut microbiome and all the bacteria, viruses, fungi and yeast that live there. Donor stool may contain disease-causing microorganisms in addition to beneficial flora. This risk is greatly reduced by screening potential donors for infectious diseases. However, typical screening will not identify uncommon viruses and unknown microorganism risks. This risk can be further reduced by using the artificial stool transplantation method.
So while fecal transplants have their advantages over antibiotics, FMT should only be considered a temporary solution. The lack of effective treatments offered by mainstream medicine pushes many people toward alternative medicine and natural remedies. Thankfully, alternatives can be very effective and safe if properly selected and used.
3 Pitfalls of Alternative Remedies
The failure of antibiotics and FMT to stop recurring infections is why people look to alternative medicine. Alternatives have many benefits but also three key shortcomings. But these shortcomings are easy to avoid if you know what they are and how to work around them.
1. Your Doctor Won’t Support YouYour doctor is unlikely to prescribe natural remedies and probably won’t support you if you choose to use alternatives. In fact, the entire mainstream medical system downplays, censors and actually fights against alternatives. The reasons for this bias against alternatives are numerous and complicated and it’s been happening for several decades. But in the last couple of years, the problem has gotten much worse.Doctors rarely deviate from standard protocol treatments and most have no training or experience with alternatives.
If you choose to use treatments outside the “standard protocol” for C. diff., then you face an uphill battle against the healthcare system. And if you want to learn more about alternatives, that information is being censored and suppressed on the internet. So if you want to use alternatives, you need to dig deep, do your own research and take a more proactive role in your healthcare. Thankfully, holistic and natural doctors offer a solution to this problem.
2. Potency and Effectiveness VaryBrowse the isles of your local health food store and you’ll see lots of isolated, single herb products. Most of these supplements are highly processed and loaded with synthetic and unnatural ingredients and fillers. Even if you find a good quality herb with high potency and minimal processing, there’s a good chance it was formulated for general health and wellness, not for strong support against stubborn C. diff. and its resistance factors, including biofilms, spores and efflux pumps.
Because there are so many supplement products available, it can hard to find the best ones simply by reading the label or the list of ingredients. One option is to get your natural remedies from a holistic or natural doctor who has a track record of treating C. difficile successfully. Another good option is to buy from a trusted source locally or online that stocks remedies used by professionals with infection patients.
3. The Overlooked Toxin Problem
C. difficile bacteria create two kinds of destructive toxins in your gut: toxin A and toxin B. These toxins cause gut inflammation, colitis, cramping and diarrhea. The more toxins the C. diff. makes, the more gut damage, diarrhea and pain you experience8.
But most natural infection remedies focus only on killing bad bacteria, not on getting rid of the toxins they produce. Toxins are also produced when biofilms inside your body break down. So failure to address toxins will slow your recovery.
New Herbal Blends for C. difficile
While C. diff. can feel like an insurmountable problem, it’s a battle you CAN win. Clearly antibiotics and fecal transplants are not the best solutions in the long term. The answer lies in new herbal remedies that combine age-old herbs in new way.
The Power of Herbal Blends

Herbal blends can attack infections on multiple fronts by combining antibacterial, immune support, tissue healing and detoxification ingredients.
For example, synergistic blends can combine antibacterial herbs, detoxification support and immune supportive substances into a single formula. Herbs that fight against C. diff. resistance factors such as spores and biofilms can also be added to the blend.
Herbs have a complex array of major, minor and trace ingredients. A single herb can have multiple modes of action. If formulated with skill and expertise, herbal blends can provide safe and effective support for the most challenging of infections.
Targeted Benefits from Specific Herbs
Below are powerful herbs that target C. diff. and it’s resistance factors. Used alone, they can be very helpful. But when blended together properly, they can unlock a wide range of healing benefits in your body.
- Garlic contains 27 known active ingredients but allicin is the best known. Allicin can interrupt quorum sensing and a recent study showed garlic inhibits C. difficile growth from spores.
- Oregano oil contains carvacrol, which reduces the number of spores that C. difficile bacteria make. Oregano also acts against efflux pumps9, L-forms stealth bacteria and biofilms10.
- Olive leaf extract has potent and broad-spectrum antimicrobial, antiviral and antifungal properties11,12. Oleuropein, a key component, protects olive trees from insects and bacteria. Olive leaf also has immune stimulating effects and anti-inflammatory properties.
- Milk thistle is a detoxification aid that also helps protect liver cells. Die-off of dead bacteria, bacterial toxins and antibiotic drugs all stress the liver, making liver support and detoxification very important for infection recovery.
- Echinacea boosts immune function by stimulating white blood cells that fight infections. It has antibacterial properties against C. diff.13 and also has antiviral properties. It also reduces inflammation.
- Cordyceps is a medicinal mushroom used for immune support and to boost energy during the recovery stage after an infection. Cordyceps promotes your immune system’s T-cell growth and helps lymphocytes to survive longer. This multi-dimensional action on the immune system can be of benefit when the body is fighting an infection.
- Goldenseal contains berberine that has immune support and tissue healing properties. This herb also inhibits C. difficile spores14, quorum sensing15 and efflux pumps16. The alkaloid content in Goldenseal stimulates the release of bile, which removes toxins from the body through the intestines. Because of it’s potent effects on the gut, goldenseal is usually blended with other herbs rather than using it by itself.







The CD Herbal Detox Kit
 The CD Herbal Detox Kit combines Michelle’s three favorite herbal blends into one kit. These blends contain the herbal ingredients detailed above, plus many others, all working together for broad, multi-dimensional support with stubborn gut infections. The Kit contains three blends that support and speed healing in different ways: Olivirex, Biocidin and GI Detox+.
The CD Herbal Detox Kit combines Michelle’s three favorite herbal blends into one kit. These blends contain the herbal ingredients detailed above, plus many others, all working together for broad, multi-dimensional support with stubborn gut infections. The Kit contains three blends that support and speed healing in different ways: Olivirex, Biocidin and GI Detox+.
Independent in-vitro laboratory sensitivity tests show that both Biocidin and Olivirex have the same range of effectiveness against multiple pathogens as some antibiotic drugs, including Ciprofloxacin, Levaquin, Sulfa and Terramycin. The GI Detox+ product absorbs C. diff. toxin A and B and helps remove bacterial and biofilm die-off debris from the digestive system.
These three blends are made by Biocidin Botanicals, a leader in specialty herbal blends since 1989. Below are some key benefits of the CD Herbal Detox Kit:
- Powerful antibacterial action. Attacks disease-causing bacteria on different fronts and with multiple modes of action.
- Targets C. difficile resistance factors, such as biofilms, efflux pumps and spore production.
- Supports the immune system in multiple ways.
- Soothes intestinal inflammation and promotes gut healing.
- High Potency. Biocidin Botanicals uses European blend herbs, which have a much higher percentage of the active ingredients than most herbal products.
- Formulated by health professionals for use by health professionals. Manufactured in GMP certified facilities in the USA. Analyzed and certified for purity and quality. FDA registered and licensed to produce nutritional supplements. Organic and wild-crafted sources are used whenever possible.
Protocol and Usage Guide
![]() The CD Herbal Detox Kit is especially formulated for gut infection support. Along with the kit you also get a detailed protocol and usage guide in Adobe PDF format. This guide will give you all the details you need to use the CD Herbal Detox Kit, including doses, precautions, instructions for children and the elderly, list of ingredients and answers to frequently asked questions. The guide can be printed or saved to your PC or mobile device.
The CD Herbal Detox Kit is especially formulated for gut infection support. Along with the kit you also get a detailed protocol and usage guide in Adobe PDF format. This guide will give you all the details you need to use the CD Herbal Detox Kit, including doses, precautions, instructions for children and the elderly, list of ingredients and answers to frequently asked questions. The guide can be printed or saved to your PC or mobile device.
We’re Here to Support You
 Our experienced staff is here to answer your questions, walk you through Michelle’s methods and provide ongoing support on your path to health. We’ll provide email support to answer any questions you may have along the way. You can also get Michelle’s free email newsletter and free probiotic video e-course.
Our experienced staff is here to answer your questions, walk you through Michelle’s methods and provide ongoing support on your path to health. We’ll provide email support to answer any questions you may have along the way. You can also get Michelle’s free email newsletter and free probiotic video e-course.
Please note: Our usage guides and information are for educational purposes and are not intended to replace a relationship with a doctor. We encourage you to make your own health care decisions based upon your research in partnership with a qualified healthcare professional.
Guarantee, Privacy and Security
We strive to provide exceptional customer service, to protect your security and privacy and to provide you with the best value and the most benefit from our products. If you are not satisfied with the CD Herbal Detox Kit, you may return new, unopened products for a refund. See our support page for details.
CD Herbal Detox Kit Special Savings
 Unlike other treatment approaches, this kit does triple duty by fighting infecting bacteria and C. diff resistance factors, boosting your immune system and soothing gut inflammation by mopping up bacterial toxins.
Unlike other treatment approaches, this kit does triple duty by fighting infecting bacteria and C. diff resistance factors, boosting your immune system and soothing gut inflammation by mopping up bacterial toxins.
With a combination of beginning and moderate usage levels, products last approximately two months. Here’s what you get:
- 1 (one) Biocidin (1 ounce bottle, approximately 600 drops)
- 2 (two) Olivirex (120 capsules total)
- 2 (two) G.I. Detox+ (120 capsules total)
Retail price is $210.85.
Order today and save $15 plus get FREE USA shipping (a total savings of $22). Special price is $195.85. This kit costs much less than most antibiotic therapies. This special is good for your first order and all future orders, while the special lasts.
** FREE Shipping on all orders over $99 **
Clicking below will take you to Michelle’s online supplement store EmbraceHealthNaturals.com.
Click here to get the CD Herbal Detox Kit today, or call us at 1-888-660-8944 to place your order (M- F, 8am – 4pm PST). Be sure to ask for the special savings on this kit.
If you have any questions, please contact us here and we’d be happy to help you.

To your very best health,

Microbiologist and Health Advocate
p.s. – Eating a low carb, low sugar diet helps starve C. diff. bacteria and it bolsters your immune system. While following the CD Herbal Detox Protocol, these dietary changes can enhance your treatment results and speed your recovery. Click here for more information on a low carbohydrate dietary approach.
* Disclaimer: Always consult with your doctor before using any new supplement or dietary change. Healthcare professionals who are experienced in using herbal medicines usually provide the highest level of support for using this protocol or other alternative methods.
These statements have not been evaluated by the US Food and Drug Administration (FDA) and they are not intended to diagnose, treat, cure, or prevent any disease.

About the Author – Michelle Moore, BSc
Michelle Moore is a microbiologist, holistic health educator, and author of C. difficile Treatments & Remedies. With over 10 years of experience in pharmaceutical research and over 20 years in natural medicine, she helps people overcome C. difficile and other chronic infections naturally.
References
- Antibiotic Resistance Threats in the United States, 2013; CDC report.
- Analysis of Clostridium difficile biofilms: imaging and antimicrobial treatment, James, G., Journal of Antimicrobial Chemotherapy, Volume 73, Issue 1, 1 January 2018, Pages 102–108.
- Espinola Lopez, Jose. Characterization of an efflux pump system, in Clostridium difficile. Thesis, 2017, Kansas State University.
- Systematic Review of Intestinal Microbiota Transplantation (Fecal Bacteriotherapy) for Recurrent Clostridium difficile Infection. Gough, E., Shaikh, H., Manges, A., Clinical Infectious Diseases 2011;53(10):994–1002.
- Long-term follow-up of colonoscopic fecal microbiota transplant for recurrent Clostridium difficile infection, Brandt LJ, Am J Gastroenterol. 2012 Jul;107(7):1079-87.
- Temporal Bacterial Community Dynamics Vary Among Ulcerative Colitis Patients After Fecal Microbiota Transplantation. The American J of Gastroenterology (2013) 108, 1620–1630 (2013).
- Fischer M, et al. Abstract 93. Presented at: Digestive Disease Week; May 21-24, 2016; San Diego 2007 Jul 14; 335(7610):80.
- Hirota SA, Iablokov V, Tulk SE, Schenck LP, Becker H et al. Intrarectal instillation of Clostridium difficile toxin A triggers colonic inflammation and tissue damage: development of a novel and efficient mouse model of Clostridium difficile toxin exposure. Infect Immun. 2012 Dec; 80(12):4474-84. Epub 2012 Oct 8.
- Jakobsen TH, van Gennip M, Phipps RK, et al. Ajoene, a sulfur-rich molecule from garlic, inhibits genes controlled by quorum sensing. Antimicrob Agents Chemother. 2012;56(5):2314-25.
- Roshan N, Riley TV, Hammer KA. Effects of natural products on several stages of the spore cycle of Clostridium difficile in vitro. J Appl Microbiol. 2018 Sep;125(3):710-723.
- Lee OH, Lee BY. Antioxidant and antimicrobial activities of individual and combined phenolics in Olea europaea leaf extract. Bioresource Technology. 2010;101(10):3751-3754.
- Perez, C. and Anesini, C. In vitro antibacterial activity of Argentine folk medicinal plants against Salmonella typhi. J Ethnopharmacol 1994;44(1):41-46.
- Hudson, J. Applications of the Phytomedicine Echinacea purpurea (Purple Coneflower) in Infectious Diseases. J Biomed Biotechnol. 2012.
- Wang S, Setlow B, Setlow P, Li YQ. Uptake and levels of the antibiotic berberine in individual dormant and germinating Clostridium difficile and Bacillus cereus spores as measured by laser tweezers Raman spectroscopy. J Antimicrob Chemother. 2016 Jun;71(6):1540-6.
- Cech NB, Junio HA, Ackermann LW. Quorum quenching and antimicrobial activity of goldenseal (Hydrastis canadensis) against Methicillin-Resistant Staphylococcus aureus (MRSA). Planta Medica. 2012;78(14):1556-1561.
- Junio H, Sy-Cordero A, Ettefagh K. Synergy Directed Fractionation of Botanical Medicines: A Case Study with Goldenseal (Hydrastis canadensis). J Nat Prod. 2011 Jul 22; 74(7): 1621–1629.