Win the Battle Against Recurring C. difficile Colitis with Remedies Your Doctor Isn’t Telling You
Microbiologist Michelle Moore’s FREE e-Book on new probiotics for gut infections is now available for instant download.
C. difficile (or C. diff.) infections cause the worst kind of diarrhea, intestinal pain, discomfort and distress. C. difficile bacteria make poisonous toxins that inflame your gut causing C. diff. colitis. Some people even have part of their intestines taken out due to this infection!
 Worse yet, C. difficile creates debilitating infections that come back again and again, robbing you of your life and comfort. C. diff. leaves you afraid of getting too far from the bathroom and dinner out with family or friends is a thing of the past. Not only are C. difficile infections resistant to antibiotics, but they are typically CAUSED by antibiotics.
Worse yet, C. difficile creates debilitating infections that come back again and again, robbing you of your life and comfort. C. diff. leaves you afraid of getting too far from the bathroom and dinner out with family or friends is a thing of the past. Not only are C. difficile infections resistant to antibiotics, but they are typically CAUSED by antibiotics.
But there’s exciting news for you today on how you can reverse C. diff. colitis, inflammation and infection so you can restore your health and get back to enjoying your life.
Doctors and Antibiotics Couldn’t Help Me
 My name is Michelle Moore and I worked in the Biotech industry as a Microbiologist and studied microorganisms for a decade. At that time, I developed my own chronic recurring infection that doctors could not help me with. I was prescribed numerous antibiotics, over and over, with no other options presented to me by my doctor. I wondered how this could happen to me, as I knew all about bacteria and antibiotics. But, antibiotics did not work. In fact, they made me worse.
My name is Michelle Moore and I worked in the Biotech industry as a Microbiologist and studied microorganisms for a decade. At that time, I developed my own chronic recurring infection that doctors could not help me with. I was prescribed numerous antibiotics, over and over, with no other options presented to me by my doctor. I wondered how this could happen to me, as I knew all about bacteria and antibiotics. But, antibiotics did not work. In fact, they made me worse.
So I had to put my education, work experience and research skills to work in order to find a better way. Thank God I found a way to resolve chronic infections that battled the infection in a different way. And, it addressed the root cause, or why the infection started in the first place.
In 2008, my husband Lester and I turned my new-found freedom into helping many others truly heal from chronic, debilitating, antibiotic resistant infections.
I won the battle and you can too! And I’m going to show you how you can win it.

“When I came down with a C. diff infection, I had never heard of it before. It was really bad — and I relapsed almost immediately after antibiotics.
Since starting Michelle’s natural protocol, I feel like I’ve finally come out the other side of this nightmare.
Honestly, I thought it might be the end of me. Thank you for giving us the information we need to regain control of our lives again.”
– Ruth, Louisiana
*Individual results may vary. This testimonial reflects a personal experience and is not a guarantee.
Why Antibiotics Fail
Perhaps you’re like most people, who went to the dentist and were prescribed an antibiotic. Or you picked up C. difficile inside a hospital. Perhaps you had some type of infection and your doctor told you to take an antibiotic for it. And before you know it, you got diarrhea and cramping that kept getting worse and didn’t go away. Next thing you know, your doctor says you have C. difficile.
C. difficile infections start because C. diff. bacteria were allowed to grow out of control. As a Microbiologist, I appreciate the communities of bacteria, like those in your gut, how they communicate with each other and they work to create balance, healthy intestines and a healthy immune system in your body.
 Just like a bountiful flower garden that has many kinds of flowers, a healthy gut is filled with all kinds of different microbes. Researchers at the Human Microbiome Project (HMP) believe we have upwards of two thousand different kinds of gut microbes. And, each type of microbe has a unique purpose, its own beauty if you will.
Just like a bountiful flower garden that has many kinds of flowers, a healthy gut is filled with all kinds of different microbes. Researchers at the Human Microbiome Project (HMP) believe we have upwards of two thousand different kinds of gut microbes. And, each type of microbe has a unique purpose, its own beauty if you will.
In a lush, vibrant flower garden, the flowers naturally crowd out and suppress the weeds. There are some weeds, but they don’t get much sunlight, space or nutrients. And, just like a lush garden, when your gut balance is healthy, your good microbes keep the bad bacteria at bay.
 However, using an antibiotic is like having a bomb going off in your garden. It kills both flowers and weeds alike. “Antibiotic bombs” kill both good and bad bacteria. Without the good bacteria in place to keep bad bacteria in check, the “bad guys” are free to start growing.
However, using an antibiotic is like having a bomb going off in your garden. It kills both flowers and weeds alike. “Antibiotic bombs” kill both good and bad bacteria. Without the good bacteria in place to keep bad bacteria in check, the “bad guys” are free to start growing.
The antibiotic created a place where the weeds now have the room and sunlight they need to grow. That is how you end up with a gut overgrowth like C. difficile.
Why C. difficile is so Hard to Treat
 Statistics show that taking an antibiotic is the number one cause getting C diff. And C. difficile is the top antibiotic resistant superbug, meaning most antibiotics have limited power to work against these bacteria.
Statistics show that taking an antibiotic is the number one cause getting C diff. And C. difficile is the top antibiotic resistant superbug, meaning most antibiotics have limited power to work against these bacteria.
One of the main problems that plagues many C. diff. sufferers is recurring infections. While antibiotics and other mainstream treatments often stop the first infection, these treatments do nothing to prevent the infection from coming back again later.
It’s critical to understand C. difficile
so you can devise a successful plan to root them out.
3 Ways C. difficile Evades Antibiotics and Wreaks Havoc
1. BiofilmsA powerful bacterial survival strategy is called a “biofilm”. C. difficile and many other bacteria build biofilms. Biofilms are clusters of microorganisms that are embedded within a tough “glue” or mineral matrix that sticks to bodily tissues, or in the case of C. difficile, adheres to the lining of the gut.Biofilms protect bacteria and make them up to 5000 times more resistant to antibiotics.
If you’ve struggled with stubborn recurring infections, there’s a very good chance that biofilms are involved. Biofilms protect the bacteria by forming a barrier against antibiotic treatments and your own immune system, creating an effective hiding place for bacteria inside your body. Biofilms also provide a “home base” from which bacteria are released into your body after antibiotic treatments are concluded.
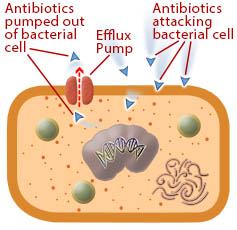
2. Efflux pumpsWhen C. difficile bacteria are exposed to a toxic compound, in this case an antibiotic, it has the ability to turn on an internal pump to remove the offending chemical. This lowers or removes the antibiotic from within the bacteria allowing it to survive during treatment. This is called an efflux pump or a Multi Drug Resistance pump inhibitor, and they also contribute to C. diff. antibiotic resistance. What would otherwise be a lethal dose of antibiotic is removed from the bacteria, allowing it to survive1.Efflux pumps expel antibiotics to prevent them from reaching a lethal concentration inside the bacterial cells.
3. Spores
Spores are a protective armor that C. diff. bacteria make, allowing them to survive treatments. You can think of a spore just like an apple seed. Seeds are able to withstand harsh temperatures and conditions until they meet soil and water and can start growing. C. difficile bacteria normally form spores as part of its life cycle.
However, when you take a heavy course of antibiotics, the drugs stress the bacteria and cause them to make spores for protection. The live bacteria may be killed by the antibiotic, but they leave their dormant spores behind. C. difficile spores can hide inside the gut, waiting until “the coast is clear” and growth conditions are right. Once your antibiotic program is over, the C. diff. can grow from the spore back into the live, active form and cause another infection.
The Case against Antibiotics
- Antibiotics cause the majority of C. diff. infections.
- Using antibiotics again and again will keep knocking down the good protective bacteria that keep C. diff. and other normal, resident microbes in check.
- Using antibiotics forces C. difficile to adapt and utilize antibiotic resistant methods like spores, efflux pumps, biofilms so it can survive.
- C. diff. is now listed at the top of the antibiotic resistant superbug infection list in the US, according to the Centers for Disease Control (CDC)2.
- Some newer antibiotics may be partially effective against biofilms or spores, but they are largely powerless against all of the ways C. difficile evades antibiotics and causes trouble 3.
- The costs can be very high for newer antibiotics that are more effective than older classes of antibiotics.
- Antibiotics kill off your good and healthy microbes (the flowers) that suppress and keep in check the normal, resident “bad” microbes (the weeds).
The Problem with Fecal Matter Transfer Treatments (FMT)
More recently, a non-antibiotic treatment is gaining popularity and availability, however many people find even after this treatment, their C. diff. infections return.
 This new procedure is called a Fecal Matter Transplant (FMT). The procedure takes stool from a healthy person’s colon (the donor) and transplants it into the colon of someone with a C. diff. infection (the recipient). Donor fecal matter can also be ingested in pill form.
This new procedure is called a Fecal Matter Transplant (FMT). The procedure takes stool from a healthy person’s colon (the donor) and transplants it into the colon of someone with a C. diff. infection (the recipient). Donor fecal matter can also be ingested in pill form.
Multiple studies have shown promising results with a cure rate around 90% as it can quickly restore good bacteria in the gut4. However, some patients relapse, require a second FMT and/or antibiotic therapy 5. FMT is simple and typically effective. However, it’s still relatively new, thus any potential long-term side effects are not known. Aside from encouraging results, it’s not all roses when it comes to FMT. Here’s some points to be aware of:
The Case against FMT
- It’s not a miracle cure. Side-effects are low, however, some people do not react well to fecal transplants. And, the procedure is not 100% effective as some still get recurring C. diff. after FMT, even without using antibiotics.
- Toxins can pass into the recipient. One study indicated that a FMT recipient’s temporary fever and elevated CRP levels (a marker for inflammation) were tied to toxins that were transferred from the donor’s fecal matter 6.
- FMT could increase your chance of recurring C. difficile infections. If you take antibiotics in the future, even if your FMT procedure was successful, there’s still a risk of getting C. diff. again. One study indicates you may have a triple risk of recurring C. diff. infection after antibiotic use7.
- Risk of exposure to unknown infectious agents. When you receive stool from a donor, you are being exposed to all of the microorganisms inside the donor’s intestines. This can be both good and bad. Scientists still know very little about the secrets of the human gut microbiome and all the bacteria, viruses, fungi and yeast that live there. The trouble is, the donor’s stool may contain disease-causing microorganisms in addition to beneficial flora. This risk is greatly reduced by screening potential donors for infectious diseases and symptoms that indicate health challenges or potential infections. However, screening will not identify less common viruses or microorganisms that can cause diseases. This risk can be further reduced by using the artificial stool transplantation method.
A Big C. diff. Problem That’s Overlooked
 Gut inflammation, swelling and diarrhea are part of the package with a C. diff. infection. This is because when C. diff. overgrows in your colon, it makes two different poisons that enable them to invade and take territory from other gut microbes.
Gut inflammation, swelling and diarrhea are part of the package with a C. diff. infection. This is because when C. diff. overgrows in your colon, it makes two different poisons that enable them to invade and take territory from other gut microbes.
They are toxin A and toxin B. The more C. diff. grows out of control, the more toxins A and B they make. The more toxins they make, the more damage, diarrhea and pain you get.
When C. diff. is managed by good microbes and they stay at normal levels in the gut, there may be little to no toxin production. However, overgrowths of C. diff. produce large amounts of toxins A and B causing severe gut inflammation and colitis, break-down of the gut lining, diarrhea, cramping and the other symptoms associated with this infection8.
Antibiotics, FMT and most mainstream treatments do not address or help against these toxic poisons being produced in the gut.
Given all the ways C. difficile evades antibiotics, and that antibiotics are the primary cause C. diff. in the first place, does it make sense to keep using these mainstream treatments against C. difficile?
The Problem with “Reseeding” Probiotics
 So if it’s all about microbial balance, then the answer must be in probiotics. Simply “reseed” good bacteria, re-establish the normal order in the gut and that will fix the C. diff. overgrowth, right? Well, the answer is yes and no.
So if it’s all about microbial balance, then the answer must be in probiotics. Simply “reseed” good bacteria, re-establish the normal order in the gut and that will fix the C. diff. overgrowth, right? Well, the answer is yes and no.
We’ve all heard about probiotics on commercials and ads. The traditional probiotic approach of ingesting probiotic strains to get them into the intestines is called “reseeding.” The idea is if you can get enough the “good guys” into your gut, they will shift the gut balance in a positive direction and that will improve your symptoms and health.
However, delivering the right strain of probiotic in enough quantity has always been a problem in the probiotic industry. The reseeding approach has many downsides and unfortunately these types of probiotics often a waste of money. Let me explain.
The Case against Probiotics
- Many probiotics are “old-school” from the dairy industry. Many Lactobacillus and Bifidobacteria probiotic strains were derived from the dairy industry. They’re used to make cheese and yogurt. They became probiotic supplements long ago, and before the recent advances in mapping the actual microbes that live in the human gut. Many of these probiotic strains have a poor track record at binding and setting up a home inside the human gut. If they are not adapted to the human gut, they will be expelled. A 2007 study showed only 38% of 11 different Lactobacillus strains were able to bind in the intestine!9
- Is the probiotic species an influencer in the gut? With recent advances in the Human Microbiome Project (HMP), it’s been discovered that all of the Lactobacillus species only make up 1% of the human gut microbiome10. That’s pretty small potatoes and you don’t hear that from probiotic manufacturers. This may be due to my next point.
- Is the probiotic species part of your unique gut microbial fingerprint? Every person has a native, unique set of microorganisms living in their gut. No two people have the same exact mixture of microbes, though there are commonalities. Your overall mixture is unique to you, just like your fingerprint. Ingesting a probiotic strain that isn’t part of your unique microbiome won’t have place to bind to and live in your gut. Unfortunately, it will just pass out of you making it a waste of money.
- Will it survive the trip through your stomach? Most probiotic supplements don’t survive the trip through the hot, highly acidic nature of the stomach. This includes Lactobacillus and Bifidobacteria strains. Your stomach is designed to be hostile in order to keep bacteria from entering your intestine. Also keep in mind, most probiotics require refrigeration to keep them alive.
- Are higher potency probiotics the answer? Higher potency probiotics (meaning higher amounts of bacteria) work to get around the hot, acidic stomach environment by delivering so many bacteria that hopefully some will make it into the intestines alive. Potency values listed on the label are at the time of manufacture. Potency values don’t account for die-off on the store shelf or during shipping or die-off going through the stomach. Getting the right species for you specifically is more important than a high potency probiotic.



As you can see, there are many downsides to traditional reseeding probiotics. The probiotic must arrive in your intestines alive and in high enough numbers and they must be part of your unique make-up in order to make a shift in your flora. The bottom line is, the reseeding approach will help some people, but certainly not everyone.
3 Steps to Win the Fight against C. diff.
Clearly antibiotics are not the best answer. And clearly traditional methods like FMT and probiotic reseeding have considerable downsides, or worse yet they may not be effective at all. The answer lies in reversing how the problem was created in the first place. Here are the three steps:
1
Cleanse C. diff. Toxins & Reduce Gut Inflammation
 Part of restoring normal gut conditions is to help quench the fires of gut inflammation caused by C. diff. toxins. This will help you feel better and will allow your intestines to start healing.
Part of restoring normal gut conditions is to help quench the fires of gut inflammation caused by C. diff. toxins. This will help you feel better and will allow your intestines to start healing.
This is often overlooked in medicine, yet it’s so simple, effective and easy to do. Novel agents can bind up C. difficile toxins A and B and escort them safely out of your colon.
My favorite probiotics in Step #2 also help destroy and remove these toxins. By removing these toxic poisons from your colon, this will ease the inflammatory immune response in your gut. This will help you feel better faster and allow healing to begin.
2
Recondition Your Gut with True Probiotics
 Get your good, health supporting microbes growing again so they can crowd out the bad guys. It’s time to get your lush flower garden growing again to crowd out the weeds.
Get your good, health supporting microbes growing again so they can crowd out the bad guys. It’s time to get your lush flower garden growing again to crowd out the weeds.
This is not traditional probiotic re-seeding. This is about reconditioning your gut. Imagine a new class of probiotics that actually work like gardeners in your flower garden. They loosen and fertilize the soil and make conditions perfect for your flowers and flower seeds to grow. Some of these gardeners can also remove the weeds.
True Probiotics Recondition the Gut and actually help because they:
- Are able to survive the harsh conditions of your stomach at 100% strength.
- Are universal in the human gut so they have a place in each person’s unique microbiome mixture.
- They will bind and colonize in the intestine of every person.
- Can shift the mixture of microbes in your gut to favorable, good and healthy species.
- Create the right conditions in your gut so that your own resident, healthy bacteria (your flowers) are restored.
- Selectively attack and kill off overgrowing, disease-causing microbes like C. difficile (see #3 below).
- True Probiotics also have a long history of human use.
3
Defend Against Bad Bacteria Using True Probiotics
 Send in “ground troops” and “snipers” to selectively target disease-causing bacteria like C. difficile and remove their toxins.
Send in “ground troops” and “snipers” to selectively target disease-causing bacteria like C. difficile and remove their toxins.
True Probiotics also police bad bacteria. One of the most exciting things about True Probiotics and C. difficile overgrowths is that some strains will actually target and eliminate overgrowing pathogens. And, some even help break down C. difficile toxins!
Targeted Precision of True Probiotics
Some of my favorite strains of True Probiotics are widely used by professionals, safe and highly effective. Here’s some of the amazing things they can do:
- Not killed by antibiotics. All strains are resistant to all antibiotics or natural antimicrobial treatments. Other probiotics are killed by these treatments.
- Reduces colon inflammation. Strains help reduce systemic inflammation and intestinal inflammation and colitis.
- Effective against C. diff. colitis. One strain is very effective at targeting colon inflammation and is effective against C. difficile colitis as well as inflammatory bowel diseases like IBS, IBD, Crohn’s and ulcerative colitis11.
- Targets harmful bacteria. Multiple strains help police the gut by producing natural antibiotic substances on site in the gut effectively targeting harmful gut bacteria.
- Inhibits C. difficile bacteria, improves C. diff. symptoms. One strain makes the antimicrobial compound clausin that directly inhibits the growth of C. difficile and other gram-positive bacteria12. It’s also been shown to improve C. diff. colitis symptoms and reduce colon inflammation.
- Targets C. diff. toxins A and B. This same strain makes an enzyme that breaks apart C. diff. toxins A and B, resulting in strong protection against intestinal damage.
- Immune system enhancement. All strains help enhance the immune system, some produce antioxidants and a broad spectrum of B vitamins inside your gut.
- Reconditions the gut. The benefits listed above all are part of reconditioning the gut. However, one strain also produces a potent form lactic acid. Think of this as fertilizer for your flower garden. It promotes the growth of native, good bacteria in your gut, including Lactobacillus and Bifidobacteria species.
- Eats C. diff. toxins. One of my favorite yeast probiotics actually digests both C. diff. toxin A and B. It reduces intestinal inflammation and controls harmful bacterial overgrowth. It also prevents the formation of C. diff. toxin B13.
Anticipate Something Amazing with a True Probiotic!
 True Probiotics stimulate the immune system, help promote gut healing, support the growth of your good bacteria and they police the gut against disease-causing overgrowths. They till and fertilize the soil of your flower garden and also pull out the weeds so they stay under control. These True Probiotics are backed by decades of human use, are widely used and studied.
True Probiotics stimulate the immune system, help promote gut healing, support the growth of your good bacteria and they police the gut against disease-causing overgrowths. They till and fertilize the soil of your flower garden and also pull out the weeds so they stay under control. These True Probiotics are backed by decades of human use, are widely used and studied.
These probiotics are truly life changing and they are one of the top 5 supplements I’ve ever used in my lifetime.
Aside from the amazing benefits of True Probiotics, there’s also a natural product that I’d also like to share with you that binds up and removes C. diff. toxins. And if you need extra support, I’ll also share some additional supportive methods that help go after C. difficile spores and break down C. difficile biofilms.
Let me help you discover a whole new world of health and healing from C. difficile with these revolutionary true probiotic strains.
Real Recovery Stories
These are real people who found hope and healing after C. diff — even when nothing else worked.
“I was sick from June to September with C. diff. After two rounds of Vancomycin, I was still running to the bathroom 20 times a day. I had almost given up. Then I found Michelle’s probiotic plan — and in two weeks, no more diarrhea. I’m still taking the probiotics. THANK YOU!”
– Sue H., Alabama
“I had terrible pain in my gut and it was unbearable at times. I took a stool test and it came back positive for Toxin a and b c-diff. With in one day of taking the stuff I could tell that it was working! I have been taking it ever since and plan on not stopping. I feel like my old self again.”
– Kristian H., Indiana
“I read all I could find and over the 4 months tried 3 different probiotics that failed to rid me of the infection. The mucus and loose stools were returning so I ordered your products. I have my life back and that is no small thing. Thank You a thousand times!”
– Tami S.
*These statements are individual experiences shared by customers. Results are not guaranteed and may vary.
Start Healing Now: Get my Free e-Book
 New Probiotics to End Gut Infections – Solutions for C difficile, SIBO, IBS, Leaky Gut and more.
New Probiotics to End Gut Infections – Solutions for C difficile, SIBO, IBS, Leaky Gut and more.
Discover how you can restore your gut and unleash the power of True Probiotics against C. difficile and other gut imbalances.
My free e-Book includes all you need to know about True Probiotics, what they do and how to get them.
We’re Here to Help
If you have any questions, please contact us here and we’d be happy to help you. I love helping people just like you discover the power of nature and tools that can restore your health from chronic infections.

Many Blessings,

Microbiologist and Health Advocate
Always consult with your doctor before using any new supplement or dietary change. Healthcare professionals who are experienced in using herbal medicines usually provide the highest level of support for using this protocol or other alternative methods.
* Disclaimer: These statements have not been evaluated by the US Food and Drug Administration (FDA) and they are not intended to diagnose, treat, cure, or prevent any disease.
References
- Espinola Lopez, Jose. Characterization of an efflux pump system, in Clostridium difficile. Thesis, 2017, Kansas State University.
- Antibiotic Resistance Threats in the United States, 2013; CDC report.
- Analysis of Clostridium difficile biofilms: imaging and antimicrobial treatment, James, G., Journal of Antimicrobial Chemotherapy, Volume 73, Issue 1, 1 January 2018, Pages 102–108.
- Systematic Review of Intestinal Microbiota Transplantation (Fecal Bacteriotherapy) for Recurrent Clostridium difficile Infection. Gough, E., Shaikh, H., Manges, A., Clinical Infectious Diseases 2011;53(10):994–1002.
- Long-term follow-up of colonoscopic fecal microbiota transplant for recurrent Clostridium difficile infection, Brandt LJ, Am J Gastroenterol. 2012 Jul;107(7):1079-87.
- Temporal Bacterial Community Dynamics Vary Among Ulcerative Colitis Patients After Fecal Microbiota Transplantation. The American J of Gastroenterology (2013) 108, 1620–1630 (2013).
- Fischer M, et al. Abstract 93. Presented at: Digestive Disease Week; May 21-24, 2016; San Diego 2007 Jul 14; 335(7610):80.
- Hirota SA, Iablokov V, Tulk SE, Schenck LP, Becker H et al. Intrarectal instillation of Clostridium difficile toxin A triggers colonic inflammation and tissue damage: development of a novel and efficient mouse model of Clostridium difficile toxin exposure. Infect Immun. 2012 Dec; 80(12):4474-84. Epub 2012 Oct 8.
- Larsen N1 Int J Food Microbiol. 2007 Feb 28;114(1):113-9. Epub 2007 Jan 17.
- Heeney, Gareau, Marco. Intestinal Lactobacillus in health and disease, a driver or just along for the ride? Curr Opin Biotechnol. 2018 Feb; 49: 140–147.
- Bacillus coagulans GBI-30, 6086 limits the recurrence of Clostridium difficile-Induced colitis following antibiotic withdrawal in mice. Leo R Fitzpatrick Gut Pathog. 2012; 4: 13
- Probiotics for Prevention of Clostridium difficile Infection. Mills J, Rao K, Young V. Curr Opin Gastroenterol. 2018 Jan; 34(1): 3–10.
- Saccharomyces boulardii protease inhibits Clostridium difficile toxin A effects in the rat ileum. Castagliuolo et al. Infect Immun. 1996 Dec;64(12):5225-32